Lumbar Spinal Fusion Surgery For Spondylolisthesis
For Back Pain Relief
Lumbar fusion surgery is a procedure performed to immobilize two adjacent vertebrae or a number of vertebrae in the lower back part of the spine. It may be performed to relieve back pain, stabilize the spine, or to restore a more normal shape to the spine.
Fusion refers to the growth of new bone between two (or more) adjacent vertebral bodies. Graft materials help to stimulate and promote this growth, acting as scaffolding across the disc space from one vertebral body to the next, thereby fusing the two vertebrae and immobilizing the spine at that segment.
A variety of bone growth-promoting materials are available to help accelerate the fusion process. In the past, bone harvested from another portion of the patient’s body was used. With the advances in technology over the past decade, there are many products that are now used to decrease the need of using the patient’s own bone.
Often surgical hardware is implanted into the spine to help immobilize the segments while the bone is fusing which can take six months to a year to occur.
Spinal fusion may be performed to relieve back pain, provide stability to the spine or to return the spine to its normal curve. When a patient is experiencing significant pain in the back, a fusion may be performed if it is determined that the pain is coming from the lumbar level.
During other situations, the surgeon may remove a significant amount of bone in order to adequately decompress nerve roots. While this extensive removal of bone will decompress the nerves and relieve pain to the legs, it may at the same time cause instability of the spine. In this case the surgeon will perform a fusion to re-stabilize the spine.
Before the operation begins, the anesthesiologist will put the patient to sleep. At this point, the positioning of the patient will depend upon which type interbody (“between vertebrae”) fusion procedure is performed. After the appropriate antibiotics are given, an x-ray may be used to guide the placement of the incision.
The numerous interbody procedures entail different approaches to the spine and different techniques used to achieve the fusion:
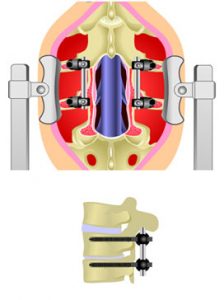
- PLIF, & TLIF – Both the PLIF (Posterior Lumbar Interbody Fusion) or TLIF (Transforaminal Lumbar Interbody Fusion) are performed on the back of the spine. The patient will be turned on to their stomach in the operating room in an extremely careful manner to protect all pressure points. The incision is performed in the midline. When performed from the back, the fusion materials may be placed on both sides of the spine (PLIF) or placed diagonally across the spine from one side (TLIF). Structural support is often placed within the interspace.
- DLIF & XLIF – A DLIF (Direct Lateral Interbody Fusion) or an XLIF (Extreme Lateral Interbody Fusion) are procedures in which the interbody fusion device is placed through an approach from the side of the patient. Again, a synthetic cage is generally placed within the interspace.
- ALIF – An ALIF (Anterior Lumbar Interbody Fusion) is a procedure to perform an interbody fusion through the front of the body by going around the abdomen.
- AXIALIF – An AXIALIF (Axial Lumbar Interbody Fusion) is a procedure to perform an interbody fusion at the bottom of the spine by placing the instruments below the sacrum and coccyx, getting to the front of the spine through a small incision behind the bottom of the spine.
- “360” Fusion – A “360 fusion” fuses both the front and the back of the spine. The front portion refers to the fusion of two adjacent vertebral bodies. The back portion fuses the transverse processes (portions of the bone which stick out of the back of the spine) or facet joints (joints which connect one spinal level to the next) of two adjacent vertebral levels. The “360 fusion” can be accomplished by making an incision and approaching from the front (through the abdomen) as well as the back, from the back only, as in the case of a TLIF, or from the side, as is done in the XLIF or DLIF.
Regardless of which type of interbody fusion is performed, screws are often used in the back of the spine to help provide rigidity while the bone fuses and grows. These screws may go through the pedicles and are known as pedicle screws. They may also go through the facet joints in which case they are called facet screws. Screws can be placed into the spine using either an open technique or a minimally invasive technique that may be performed through small incisions in the skin.
Posterolateral Fusion – Often the surgeon may also perform a posterolateral fusion. During this procedure, the surgeon lays bone along the back and side of the spine with the intent that this portion of the spine will also grow together.
Patients have generally discharged home anywhere from one to four days following surgery. Patients may be instructed to wear a back brace post-op. They will be advised to avoid bending, twisting or lifting for several months. This is necessary to allow the fusion to properly heal.
The pain in the leg is typically significantly improved, although the patient may experience numbness in the leg, twinges of leg pain, pain around the incision and, at times, spasms of the back muscles. Medications will be given for this. This should improve within one to two weeks after surgery.
Patients might experience back pain and spasms following surgery, but this should improve in the first week or two after the procedure. Patients should keep their back incisions dry until they are seen in the office generally seven to ten days after surgery. Return to work will be addressed on an individual basis depending upon the requirements of the patients’ work duties.
Potential risks include bleeding, infection, nerve injury, spinal fluid leak and recurrence of another disc herniation at the same level. There is also the possibility that the fusion may not take and that persistent mobility can occur. This is known as pseudarthrosis.